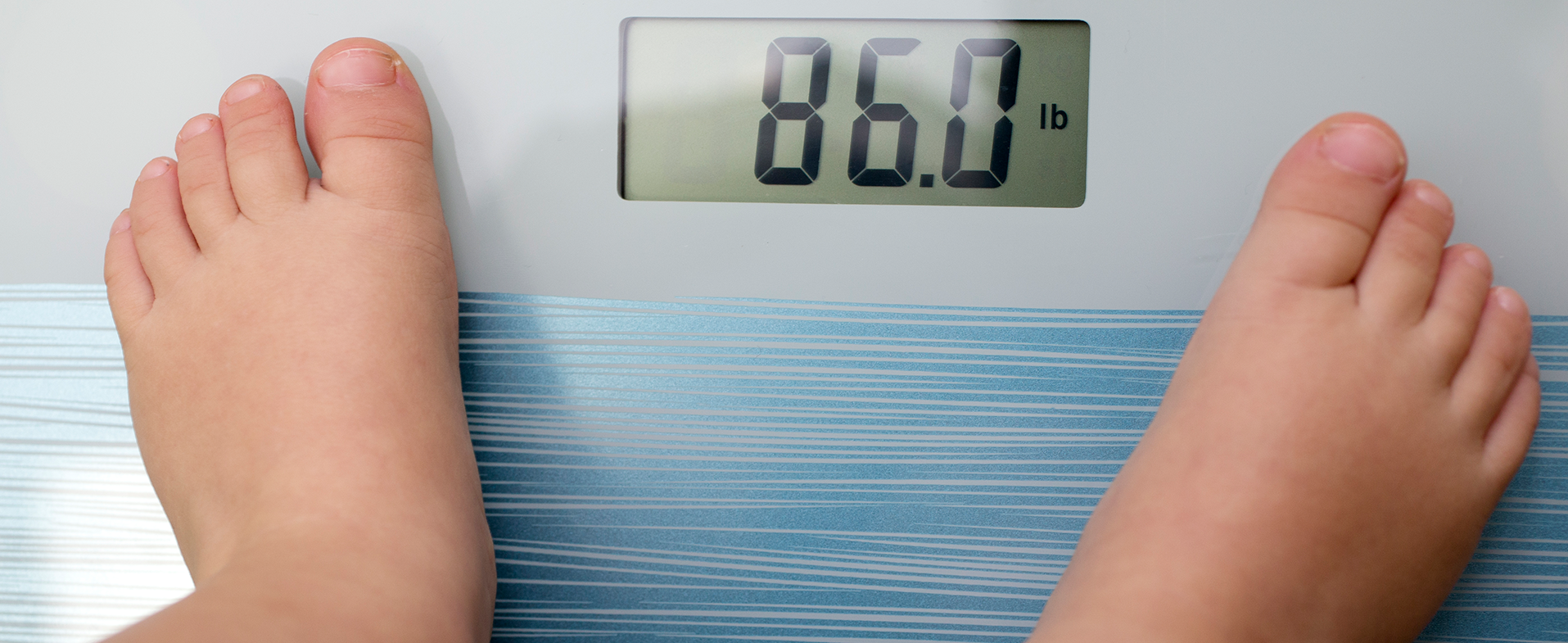
Nearly one in five children ages 10 to 17 in Michigan are considered obese, reports the Robert Wood Johnson Foundation, and about one in three are overweight, says the United Health Foundation.
“We are not only seeing the rate of obesity increasing in older children and adolescents, but also in children younger than six years of age,” says Uzma Shah, M.D., chair of pediatrics at Henry Ford Health. “And perhaps even more concerning is that in addition to this, levels of severe obesity are climbing to higher BMIs.”
A child is considered overweight when their BMI (or body mass index) falls within the 85th and 95th percentiles and obese when their BMI falls in the 95th percentile or above.
Treatment Intervention For Childhood Obesity
The Centers for Disease Control & Prevention (CDC) organizes childhood obesity into three classes, with class three being linked to the greatest amount of health complications, such as high blood pressure, high cholesterol, cardiovascular disease, Type 2 diabetes, osteoarthritis, fatty liver disease and sleep apnea. While these health conditions are more common in adults, having obesity as a child can cause them to develop at earlier ages.
Because of this, the American Academy of Pediatrics (AAP) has developed guidelines for the use of four FDA-approved weight-loss drugs – Wegovy, Saxenda, orlistat and Qsymia – in children ages 12+ who are severely obese. These medications reduce appetite and increase the feeling of fullness. Side effects can include nausea, vomiting, diarrhea, stomach aches and headaches.
“The AAP guidelines are very clear and don’t allow for immediately jumping to weight loss medication,” says Dr. Shah. “Healthy lifestyle intervention is first, which you have to try for at least six months. At Henry Ford, this consists of the Healthy Weight Clinic, a CDC-recognized program that offers intensive health behavior lifestyle treatment. The child and their parents will meet with a special team composed of a hepatologist, gastroenterologist, dietitian and psychologist to address all aspects of obesity, such as nutrition, exercise, genetic factors and mental health. When it comes to any childhood medical condition, you’re not just treating the condition – you’re helping the child and their family.”
Healthy Weight Clinic
Participation in the clinic has been shown to reduce BMI, parental stress and binge eating symptoms, and improve quality of life for patients and their families. Patients and families receive tailored support, including medical management of obesity-related comorbid conditions, like sleep apnea, hypertension and diabetes, along with any other chronic conditions like asthma and ADHD.
An obstacle, however, arises from the fact that healthy lifestyle intervention is pretty intensive: it involves a family commitment of about 26 hours per week for about three to 12 months, which some families may not be able to take on. Other families may not even know about the resources available to them - especially those in lower socioeconomic brackets, where childhood obesity is more common and there is limited access to healthy foods and healthcare centers of excellence.
Yet for children who do make healthy lifestyle changes, if they have severe obesity, additional interventions may be necessary.
“If healthy lifestyle changes aren’t enough, a child who has severe obesity can be considered for medications in a very controlled circumstance,” says Dr. Shah. “And if that ends up not being enough, they can be considered for bariatric surgery. But this is only after ensuring all considerations have been properly evaluated by a specialized team.”
Reviewed by Uzma Shah, MD, FAAP, FAASLD, chair of pediatrics at Henry Ford Health. She specializes in pediatric gastroenterology and nutrition, pediatric hepatology, pediatric pancreatology and pediatric transplant hepatology.