Study Shows Antibiotics May be Viable Option for Appendicitis Instead of Surgery
DETROIT – Every year more than 250,000 people undergo surgery for appendicitis, making it one of the 20 most common surgeries performed in the United States.
In the largest randomized U.S. study of appendicitis published today in the New England Journal of Medicine, researchers from Henry Ford Health System and 24 other sites around the U.S. report that seven in 10 patients who received antibiotics avoided surgery and that patients who took antibiotics for symptom relief fared no worse in the short term than those who underwent surgery.
Still, researchers cautioned that taking antibiotics for appendicitis is not for everyone and advised patients to consult with their physician.
“The significance of this study means that surgeons and patients now have more options for the treatment of appendicitis,” says J.H. “Pat” Patton, M.D., medical director of Surgical Services for Henry Ford Health System and a study co-investigator. “We now know that we can safely and effectively treat a significant number of patients with antibiotics alone and avoid surgery. We encourage patients to weigh their options based on their individual circumstances before deciding which treatment is best for them.”
Henry Ford was among 25 U.S. sites in 14 states that participated in the study, Comparing Outcomes of Antibiotic Drugs and Appendectomy (CODA). With 1,552 patients studied between May 3, 2016 and Feb. 2, 2020, CODA represents the largest study comparing surgery and antibiotics in adults with appendicitis and is roughly three times larger than the previous one. The study was funded by the Patient-Centered Outcome Research Institute.
Unlike prior studies, CODA was the first to include patients with severe appendicitis and a condition called appendicolith, in which a small stone forms in the appendix. Researchers originally planned to report their findings after patients recovered for one year. With concern about limiting unneeded surgeries during the height of the COVID-19 pandemic, researchers decided to reduce the time frame for reporting results following either surgical or antibiotic intervention to 90 days in order to give physician data on the effectiveness of this non-surgical option.
Key findings of the study:
- Seven in ten patients who received antibiotics avoided surgery within the first 90 days following treatment, while three in ten did eventually need surgery within the same time frame
- Four in ten patients with an appendicolith who received antibiotics required surgery within 90 days of receiving antibiotics as their first treatment
- Patients treated with either antibiotics or surgery experienced symptoms of appendicitis for about the same amount of time prior to treatment
- Patient treated with antibiotics missed less time from work or school but reported more visits to the Emergency Department and days spent in the hospital overall than those who had surgery
Researchers acknowledge that the study’s timing in the middle of a pandemic could have broad implications for both patients and hospitals. Risk of COVID-19 exposure or going to a hospital continues to be a real concern for patients who may find antibiotic treatment a preferred choice. The study also provides hospitals with clarifying options as they prepare for a possible surge of COVID-19 cases this fall and winter. Because of health care disparities highlighted in the pandemic, Dr. Patton cautions that doctors be mindful of properly addressing vulnerable patient populations on the implications of the study.
“We recognize some patients may not want to come into a hospital environment during a pandemic. This study tells us that antibiotics are a viable option for some of these patients,” Dr. Patton says. “And as the data are starting to show, patients who are COVID positive and undergo general anesthetic may have more complications than they may otherwise have. If we can treat patients successfully on an outpatient basis, we can keep them out of the hospital and preserve resources for other types of surgeries.”
Jeffrey Johnson, M.D., medical director of Trauma at Henry Ford Hospital and co-investigator on the CODA trial, recommends that patients assess all their options with their doctor.
“Beyond the treatment itself, patients need to fully explore their medical condition and personal factors like time off from work and school, insurance coverage and caregiving responsibilities when making their decision,” Dr. Johnson says. “What this study shows is there is no one-size-fits-all approach. Patients ought to evaluate the benefits and risks of taking antibiotics or opting for surgery and make an informed decision on what is important to them.”
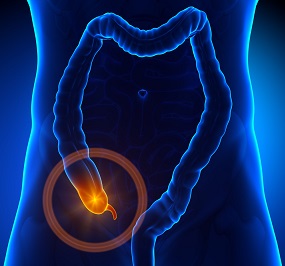
An appendectomy is the standard treatment for treating appendicitis and most patients recover quickly and without complications. The procedure is performed laparoscopically or by one incision and involves surgically removing the appendix, a small tube-shaped pouch that is attached to the large intestine in the lower right side of the abdomen. Severe abdominal or stomach pain, low-grade fever and loss of appetite are classic symptoms. An overnight hospital stay is typical for most patients.
In the study 776 patients were randomly assigned to receive antibiotics and 776 patients to undergo appendectomy (776). Patients’ median age was 38 and 63 percent were men and 37 percent women. The ethnic background was 60 percent white, 23 percent other, 5 percent Asian, 2 percent American Indian or Alaska Native and 1 percent Native Hawaiian or Pacific Islander.
Patients in the antibiotics group received a 10-day course of antibiotics based on guidelines from the Surgical Infection Society and Infectious Diseases Society of America.
Of the 1,552 patients, 172 were enrolled at Henry Ford Hospital, the health system’s hospital in Detroit.
Researchers will be reporting on additional findings from data that continues to be collected from patients. Future analysis will examine long-term quality of life, recurrence of appendicitis in the antibiotics group and predictors of outcomes based on patient characteristics among other topics.
###
MEDIA CONTACT: David Olejarz / David.Olejarz@hfhs.org / 313.303.0606
About Henry Ford Health System
Founded in 1915 by Henry Ford himself, Henry Ford Health System is a non-profit, integrated health system committed to improving people’s lives through excellence in the science and art of healthcare and healing. Henry Ford Health System includes six hospitals including Henry Ford Hospital in Detroit; Henry Ford Macomb Hospitals; Henry Ford Wyandotte Hospital; Henry Ford West Bloomfield Hospital; Henry Ford Allegiance in Jackson, MI; and Henry Ford Kingswood Hospital – an inpatient psychiatric hospital.
Henry Ford Health System also includes Henry Ford Medical Group: Henry Ford Physician Network; more than 250 outpatient facilities; Henry Ford Pharmacy; Henry Ford OptimEyes; and other healthcare services. Our not-for-profit health plan, Health Alliance Plan – HAP – provides health coverage for more than 540,000 people.
As one of the nation’s leading academic medical centers, Henry Ford Health System trains more than 3,000 medical students, residents, and fellows annually in more than 50 accredited programs, and has trained nearly 40% of the state’s physicians. Our dedication to education and research is supported by nearly $100 million in annual grants from the National Institutes of Health and other public and private foundations.
Henry Ford Health System employs more than 33,000 people, including more than 1,600 physicians, more than 6,600 nurses and 5,000 allied health professionals. For more information, go to henryford.com
.svg?iar=0&hash=F6049510E33E4E6D8196C26CCC0A64A4)

/hfh-logo-main--white.svg?iar=0&hash=ED491CBFADFB7670FAE94559C98D7798)