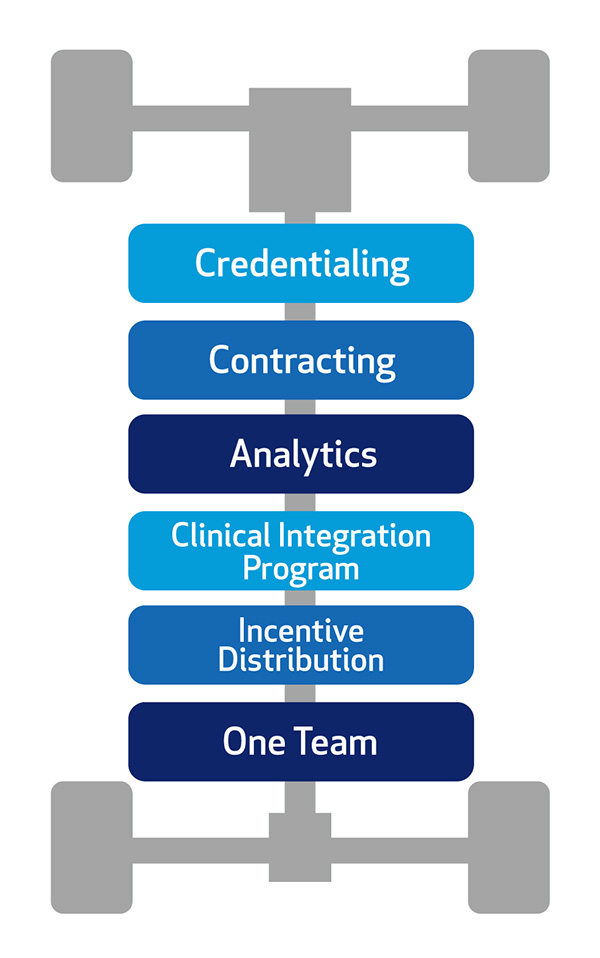
What You Gain with Mosaic CIN
A Unified Best-In-Class Clinical Integration Program
 Mosaic CIN’s Clinical Integration Program powers our value-based care strategy—merging evidence-based practices with a performance-focused model that improves population health and advances the Quintuple Aim.
Mosaic CIN’s Clinical Integration Program powers our value-based care strategy—merging evidence-based practices with a performance-focused model that improves population health and advances the Quintuple Aim.
Key features include:
- Aligned incentives: Uniting goals across patients, providers and payors.
- Clear metrics: Measuring quality and cost performance to track progress.
- Quarterly scorecards: Delivering timely insights at the network and physician levels.
This unified model enhances our ability to secure value-based contracts and recognize providers for delivering high-quality, cost-effective care.
-
Contracting
Mosaic CIN employs a network-wide contracting strategy that establishes clear, performance-based targets. Full participating members benefit from our negotiated professional and facility payor contracts, emphasizing value-based reimbursement.
We engage with Commercial, Medicaid, Medicare Advantage plans, and local employers.
The CIN generates incentive payments for eligible members by driving improved quality and cost savings. Our collective negotiations align reimbursement rates, performance incentives, and value-based terms to support the Quintuple Aim.
-
Credentialing
Mosaic CIN simplifies credentialing by centralizing and coordinating the process across contracted health plans. Instead of navigating payor-by-payor enrollment, providers complete a single, unified credentialing process every two years.
With delegated credentialing agreements in place for 80% of our health plans, we reduce administrative burden, accelerate enrollment, and support efficient revenue cycle management — ultimately lowering operational costs.
-
Analytics
Mosaic CIN provides meaningful, actionable data through a unified scorecard system that drives improvement and supports value-based performance. Community and individual scorecards track progress toward shared goals and highlight each provider’s contribution.
Because payors have adopted our scorecard as the single source of truth, practices can align their efforts around one consistent set of metrics. These metrics focus on six key performance areas — ranging from prevention and chronic care to coordination, efficiency, patient experience, and professional engagement — ensuring a clear path toward delivering better outcomes across the network.
-
Clinical Integration Program
Mosaic CIN’s coordinated strategy advances outcomes, efficiency, and equity.
- Our population health and health equity initiatives focus on patients with complex medical, behavioral, and social needs.
- A dedicated team of nurse care managers and community health workers helps reduce hospitalizations and crisis-driven care while improving quality of life and long-term outcomes.
- Our Community Health Technology Network enhances coordination by connecting providers through a shared Epic EHR platform. Integrated with Henry Ford Health, this system links primary care, specialists, hospitals, urgent care centers, and surgery centers—ensuring seamless, data-informed care across the continuum.
-
Incentive Distribution
Shared savings, performance incentives, and advanced payments align effort and reward across the network.
Members may earn incentive payments, per-member-per-month (PMPM) funds, shared savings, and fee schedule enhancements through Mosaic CIN’s value-based payor contracts.
-
One Team
A dedicated team supports practice success, performance improvement, and value creation at every level.
Each practice is paired with a liaison who meets regularly with office leadership to provide quality and utilization support, share payor updates, and review contract performance. These collaborative meetings focus on high-impact activities, with planning and accountability built in to drive results. Members also benefit from proven best practices that elevate individual and network performance.
Our Community Health Technology Network further enhances coordination through a shared Epic EHR, fully integrated with Henry Ford Health. This connectivity links primary care, specialists, hospitals, urgent care centers, and surgery centers, ensuring seamless care across the continuum for shared patient populations.
