Kyleisha’s Story
A pacemaker at 25. Heart failure at 27. An LVAD implant shortly after. It was a lot, but with support from her family and Henry Ford team, this mother of four can now focus on what matters most.
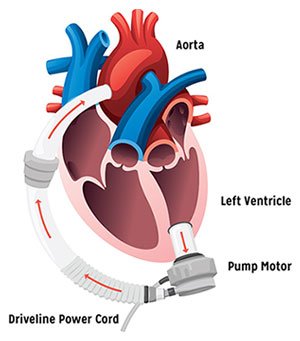
An LVAD features several key components, which work together to improve heart failure symptoms.
 Ventricular assist devices, or VADs, are permanent heart pumps that support the severely failing heart. The pump works with your heart to deliver blood to your organs, improving breathing, energy and swelling, and increasing your chances of survival.
Ventricular assist devices, or VADs, are permanent heart pumps that support the severely failing heart. The pump works with your heart to deliver blood to your organs, improving breathing, energy and swelling, and increasing your chances of survival.
When this supports the left side of the heart, it’s called an LVAD. This is the most common type of VAD implant.
When the heart’s natural pumping function is severely weakened, it is not able to deliver blood to your organs and muscles. This is why people with heart failure can feel many symptoms, including shortness of breath, tiredness, weakness, swelling and bloating:
The LVAD support system is composed of several key components both inside and outside your body, including:


Living with an LVAD will come with changes and you will have to adjust to a “new normal.”
This sounds like a lot and may be overwhelming, but in many cases, people on LVAD supports become experts at managing their LVAD equipment and driveline within a few months.

A pacemaker at 25. Heart failure at 27. An LVAD implant shortly after. It was a lot, but with support from her family and Henry Ford team, this mother of four can now focus on what matters most.
Your Henry Ford LVAD team is here to support you. We begin training family members prior to surgery, and will not send you home until we feel you can safely manage your LVAD support system. In addition, we are there 24/7 to answer any questions you have after being discharged from the hospital.
You can also read our patient stories to see how others have lived on LVAD support, and learn more about screening to determine if you’re eligible for an LVAD, the surgical process and important life changes you’ll need to make. If you would like to meet an LVAD patient, we can often arrange this as well.
Despite the real risk for complications and the potential lifestyle challenges, most people thrive after LVAD support. Over time, most people have less shortness of breath and have more much more energy than prior to LVAD surgery.
For some people, LVAD support will not fully address severe heart failure. We offer other surgically implanted mechanical heart support devices for people with complex heart problems:
We use cookies to improve your website experience. By using this site, you agree to our Terms of Use. Read our Internet Privacy Statement to learn what information we collect and how we use it.