From Traverse City to Detroit to Siesta Keys in Florida — and back again — Bob Robinson hasn't missed a beat following lung cancer treatment.

After a pancreatic problem was resolved, Bob Robinson was just following doctor’s orders to have a PET scan taken every six months in Traverse City. That’s when he learned he had a spot on his lung. “It was a luck thing. I was very fortunate they picked it up at that early stage,” says Bob Robinson, a 72-year-old Traverse City resident.
“Come down here to Detroit, and let’s take care of this,” said David Kwon, M.D., surgical oncologist at Henry Ford Cancer.
This wouldn’t the first time that Bob had seen the inside of a Henry Ford operating room. Four years earlier, an intraductal papillary mucinous neoplasm on his pancreas launched a hunt for the best doctor to treat it. “I did my research and learned that Dr. Kwon was the top dog in the state for doing a WHIPPLE procedure that I needed,” says Bob. “So I felt confident with him.”
Now, it was time for confidence to expand.
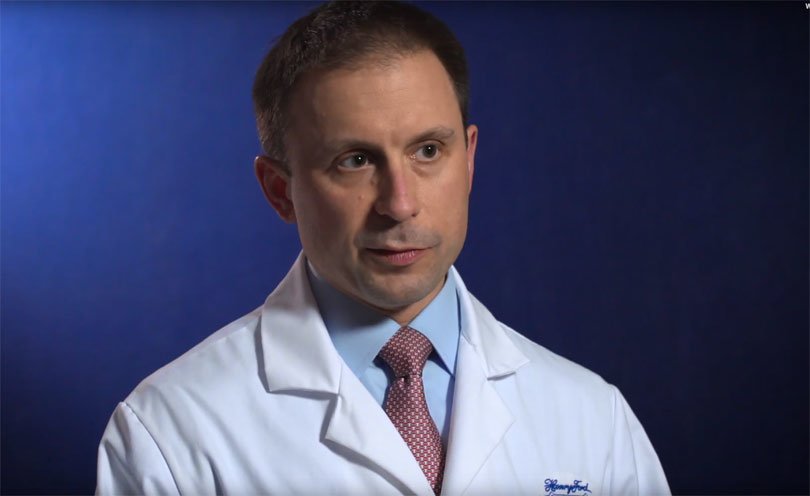
Andrew Popoff, M.D., thoracic surgeon at Henry Ford was called in and became part of Bob’s multidisciplinary team. He studied the scan taken by the PET mobile unit in Traverse City and confirmed what Bob had feared. “I’d have to have it removed,” says Bob, a former electrical contractor who currently builds storage units for travel homes and other recreational vehicles in Michigan.
“Bob had a nodule between the upper and lower lobes in the left lung. The nodule was on top of the main artery to the left lung. It was unclear whether or not this was related to the intraductal papillary mucinous neoplasm. But the bottom line was — it looked highly suspicious,” says Dr. Popoff.
To remove the nodule, Dr. Popoff performed video-assisted thoracoscopic surgery (VATS). The minimally invasive procedure involves inserting a tiny camera, called a thoracoscope, through a small incisions in the chest.
Imaging showed that the lymph node was stuck onto the pulmonary artery, so freeing the nodule from the artery was challenging. “It’s a big blood vessel with a lot of flow through it. But we were able to do it safely,” says Dr. Popoff.
Lung cancer usually spreads from a tumor in the lung to the nearby lymph nodes. However, Bob only had cancer in the lymph node, not in the lung. Bob’s situation is unusual in that there was no readily identifiable primary tumor, as is typical in lung cancer.
“I anticipated some pain, but that didn’t happen. I was pleasantly surprised,” says Bob. He stayed in the hospital for one night and then went to his daughter’s home nearby in Detroit before he headed Up North. Bob also has two grown sons who live outside of Michigan. He and his wife, a former nurse, are from families that have spent three generations in Traverse City.
“I was sitting in my office a week later doing work, and I never felt pain — absolutely no pain,” says Bob.
Says Dr. Popoff: “Pain in subjective. Typically, people don’t have the experience of no pain like Mr. Robinson. They have some, but we manage it. Still, when you compare the amount of pain, length of stay and functional status with minimally invasive surgery to traditional open approaches, then hands down, minimally invasive wins every time. That’s why we do it. Not that it’s easier for the surgeon — it’s actually harder. It’s easier to just make a big incision. But we do minimally invasive surgery because it makes a huge impact on the patient’s quality of life.”
 At Henry Ford, the approach to chest surgery and lung cancer is to do the operations minimally invasively. Each year, about 90 percent of them are performed minimally invasively. In addition to having less post-operative pain and a shorter hospital stay, patients have an earlier return to normal activity. Otherwise, their hospital stay could be five or more days, which makes a big difference for people.
At Henry Ford, the approach to chest surgery and lung cancer is to do the operations minimally invasively. Each year, about 90 percent of them are performed minimally invasively. In addition to having less post-operative pain and a shorter hospital stay, patients have an earlier return to normal activity. Otherwise, their hospital stay could be five or more days, which makes a big difference for people.
“It’s amazing — the surgeries they can do today and not be that invasive,” says Bob. “The whole team at Henry Ford was outstanding. Both of the doctors I worked with had excellent teams. Each did their separate work, but they all knew what was going on. It wasn’t like only one person knew and the others didn’t. It was a very well-organized team, and the whole experience was very good,” says Bob.
Traveling back and forth from Michigan to Florida hasn’t been a problem for Bob. He says he can call his doctors from either place and they respond quickly.
“Mr. Robinson was a great patient and his wife was very supportive. They were fantastic people to work with,” says Dr. Popoff.
These days, Bob exercises a little more and eats a little better. “Although I didn’t have too many bad habits with eating,” says Bob who quit smoking five years ago. “I’m going to keep making storage buildings. I’ll see my kids and grandkids a lot in the summer in Northern Michigan, and I’ll take a little more time in my condo down here in Florida,” says Bob. He speaks as if he’s a lucky guy who is just a short walk from the fine white sands and relaxing, warm breezes on the beach of Siesta Key, or the shoreline of lake Michigan. And he is.
.svg?iar=0&hash=F6049510E33E4E6D8196C26CCC0A64A4)

/hfh-logo-main--white.svg?iar=0&hash=ED491CBFADFB7670FAE94559C98D7798)

 At Henry Ford, the approach to chest surgery and lung cancer is to do the operations minimally invasively. Each year, about 90 percent of them are performed minimally invasively. In addition to having less post-operative pain and a shorter hospital stay, patients have an earlier return to normal activity. Otherwise, their hospital stay could be five or more days, which makes a big difference for people.
At Henry Ford, the approach to chest surgery and lung cancer is to do the operations minimally invasively. Each year, about 90 percent of them are performed minimally invasively. In addition to having less post-operative pain and a shorter hospital stay, patients have an earlier return to normal activity. Otherwise, their hospital stay could be five or more days, which makes a big difference for people.