A Second Wind
By the time he retired, Tom Aldridge had experienced a series of life-threatening health problems.
 “When I was younger, I was in pretty good health,” says Tom, 66, a retired sales engineer and resident of Swartz Creek, near Flint. “But I had been a smoker, and all of my recent health issues led back to my 40 years of smoking.”
“When I was younger, I was in pretty good health,” says Tom, 66, a retired sales engineer and resident of Swartz Creek, near Flint. “But I had been a smoker, and all of my recent health issues led back to my 40 years of smoking.”
It started with a diagnosis of chronic obstructive pulmonary disease (COPD), followed by an abdominal aortic aneurysm. Then, Tom had a heart attack and double bypass surgery. This worsened his COPD and Tom needed to go on oxygen, but after attending a local pulmonary rehabilitation program he was able to stop using it.
In 2020, Tom went into the hospital with chest pains, and his local team did a full heart attack workup. It turned out to be COVID-19. However, while he was waiting to be transferred to the COVID unit, he went into cardiac arrest.
“They worked on me for about 15 minutes to bring me back,” Tom says. “COVID definitely put me over the edge. After this, I was put on oxygen full-time.”
While Tom had a personal history of smoking that helped to drive these health issues, he also had a strong family history.
“All of my grandparents died from some form of cancer,” he says. “My dad was a smoker and developed cancer. My sister was a smoker and had COPD and cancer, and she passed away at 59. My older brother had his first heart attack at 34, and he passed away a couple of months ago.”
 Slowing Down
Slowing Down
At a certain point, Tom was also diagnosed with emphysema, a specific type of COPD that is characterized by progressively increasing breathlessness.
As his breathing issues got worse over the years, Tom experienced some limitations.
“I always worked on my own cars,” he says. “I remember doing a brake job for my daughter’s car. I was down on the ground compressing my lungs, and what should have taken 45 minutes took me over three hours.”
He also missed bowling.
“After my heart bypass surgery, my wife and I joined a church league,” Tom says. “I got a sense of how bad my lungs really were when I had to buy a lighter ball.”
And after his bout with COVID, Tom and his wife couldn’t go camping anymore.
“We had a motor home, but I struggled to tear it down, so we sold it,” Tom says.
While going through his local pulmonary rehab program for a second time, he learned about Henry Ford Health’s Pulmonary program.
“A couple of the respiratory therapists had been to a seminar at Henry Ford and recommended that I check out their program,” Tom says.
A Good Candidate
 In his first appointment at Henry Ford Hospital in Detroit, Tom met with Michael Simoff, M.D., Rebecca Priebe, NP and other Pulmonary team members.
In his first appointment at Henry Ford Hospital in Detroit, Tom met with Michael Simoff, M.D., Rebecca Priebe, NP and other Pulmonary team members.
“They did a bunch of testing, and when the results came back they told me I was a good candidate for the BLVR procedure,” Tom says.
BLVR (bronchoscopic lung volume reduction) is a minimally invasive procedure that places tiny Zephyr® Valves in a person’s airways in the most diseased lobe of the lungs to treat advanced emphysema. Zephyr Valves are the first FDA-approved, device available in the U.S. for treating patients with severe emphysema.
“I had done some research on the procedure and different hospitals even before they told me about it, and I knew Henry Ford was the right place for me,” Tom says.
When they met to discuss the procedure, Tom’s care team told him about some of the cases they had done, and what to expect. These one-way valves are placed under general anesthesia and the procedure typically is completed in under an hour. Using a bronchoscope, doctors will place an average of 3-5 valves in airways to allow the trapped air in that lobe to escape but prevent new air from getting trapped. This allows the treated lobe to deflate and the diaphragm to expand improving breathing capability.
The clinical team explained to Tom that they were targeting the left upper lobe of his lung, because they felt this would be the best option for the procedure.
“My expectations were high,” Tom says. “I let everyone know upfront that my goal was to get off of oxygen, but they let me know there was no guarantee this would be possible.”
Surgery and Recovery
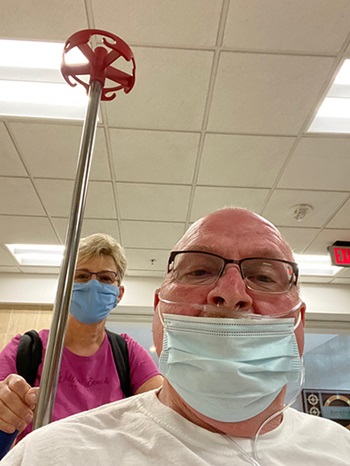
 The morning of the procedure, the couple walked over to the Henry Ford entrance from the hospital apartments where they stayed, and Tom had his surgical prep.
The morning of the procedure, the couple walked over to the Henry Ford entrance from the hospital apartments where they stayed, and Tom had his surgical prep.
“I met with the staff, and Dr. Simoff came in with the anesthesiologist and the rest of the team,” Tom says. “I told my wife I’d see her in a few hours, and they took me away. She was nervous, but I had faith everything would go well.”
When Tom woke up in the ICU he was still on oxygen, but he noted to his wife that his breathing was already a little easier.
Tom’s care team told him they would have him get up and move around, and that they were watching for any potential issues, such as spitting up large amounts of fluid from his lungs, or a collapsed lung (also known as pneumothorax).
“They also told me that due to my anatomy, they had placed additional Zephyr valves in my airways, a total of seven,” Tom says.
Tom stayed the full four days in the hospital, all in the ICU.
“Normally they would transfer you out of the ICU as you improved, but because of COVID, they didn’t have any beds,” Tom says. “The staff there was fantastic, although they didn’t know what to do with me, because I felt so good. Definitely not the typical ICU patient.”
 Tom was up and walking the day after his procedure, and he pushed himself.
Tom was up and walking the day after his procedure, and he pushed himself.
“I would walk until my oxygen levels dropped, then sit down and recover,” he says. “I was determined to get stronger. I was still on oxygen, but I could breathe easier.”
Once he returned home, Tom had some periodic follow-ups with his care team.
“One month out, I was already reducing my oxygen usage and it got even better at six months,” Tom says. “During my 6 month pulmonary function testing, my lung function was at 36%, up from 24% prior to the BLVR procedure. That’s a 50% improvement.”
However, just before his 1-year follow-up, Tom came down with pneumonia and was readmitted to the hospital.
“My wife was worried that this would affect my recovery,” Tom says. “When I got out of the hospital and had my 1-year follow-up, my levels were about the same as they were at six months, but if I hadn’t come down with pneumonia, they probably would have been even better.”
Back to Enjoying Life
 “I still like to push myself,” Tom says. “My wife gets worried about me, because she lost her first husband when she was young, and she’s worried about that happening again. At the same time, she saw how quickly I recovered from the BLVR procedure as opposed to previous ones, and she’s seen the improvement in me.”
“I still like to push myself,” Tom says. “My wife gets worried about me, because she lost her first husband when she was young, and she’s worried about that happening again. At the same time, she saw how quickly I recovered from the BLVR procedure as opposed to previous ones, and she’s seen the improvement in me.”
Their four adult children have also seen improvement in Tom’s health and have been very encouraging.
“They were also a little nervous about my BLVR procedure, but supportive,” Tom says. “Our oldest daughter is 42 and has had asthma all of her life, so she understood my struggles with breathing.”
These days, there are times when Tom can go completely without oxygen if he’s not doing anything physically straining. At other times when he is being physically active, he uses a pulse oximeter to test his oxygen levels, and he sits down and uses oxygen when his levels drop or he feels winded.
“My doctors want me to keep my oxygen saturation level above 90 at all times,” Tom says. “I’ve learned to know when my body needs it. And now I can do more. I can still maintain some independence. When I want to mow our lawn, I have a portable oxygen that I can carry in a backpack. And while I don’t work on cars anymore, I could.”
Earlier this year, Tom and his wife also bought another camper, and they’re planning a major camping trip. In addition, Tom has his eye on a return to bowling.
He’s grateful for the Pulmonary team at Henry Ford for helping him reduce his dependency on oxygen and get his life back.
“I’m a man of faith, and I believe if it’s meant to be it will happen,” Tom says. “God led me to Henry Ford, and I’m so thankful for everything they’ve done for me. They love what they’re doing, and they care for their patients. Everyone was fantastic throughout. They managed my expectations upfront, encouraged me throughout the process and have been there for me anytime I’ve needed them.”
.svg?iar=0&hash=F6049510E33E4E6D8196C26CCC0A64A4)

/hfh-logo-main--white.svg?iar=0&hash=ED491CBFADFB7670FAE94559C98D7798)